Knee Injury Guide
COMMON INJURIES
> Patellar Tendonitis (Jumper’s Knee)
General Information
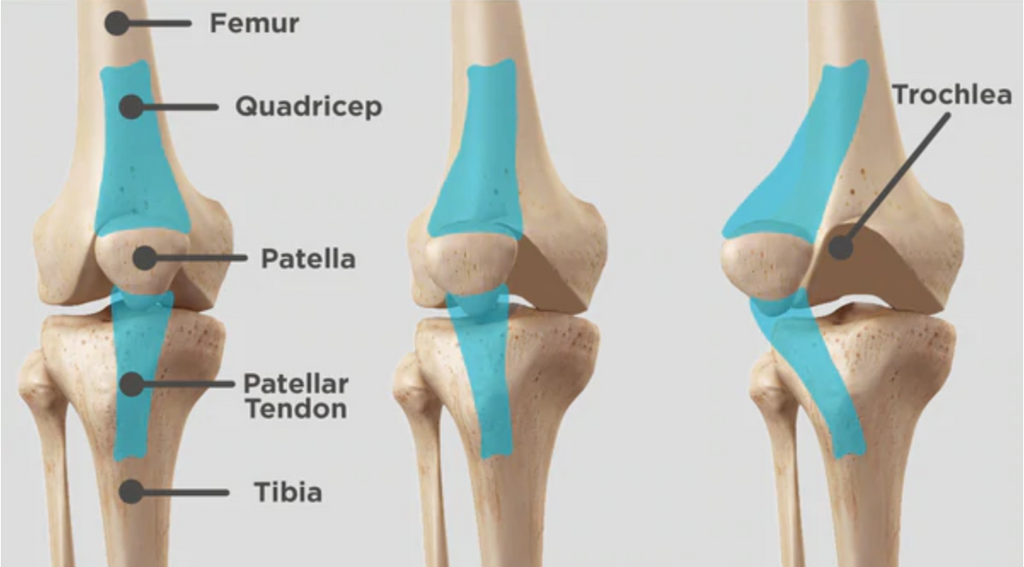
Jumper's knee, also known as patellar tendonitis, is a condition characterized by inflammation of your patellar tendon. This connects your kneecap (patella) to your shin bone (tibia). Jumper’s knee weakens your tendon, and, if untreated, can lead to tears in your tendon.
Jumper’s knee is caused by overuse of your knee joint, such as frequent jumping on hard surfaces.
It’s usually a sports-related injury, linked to leg muscle contraction and the force of hitting the ground. This strains your tendon. With repeated stress, your tendon may become inflamed.
COMMON SYMPTOMS:
Following are the most common symptoms of jumper's knee. However, you may experience symptoms differently. Symptoms may include:
- Pain and tenderness around your patellar tendon
- Swelling
- Pain with jumping, running, or walking
- Pain when bending or straightening your leg
- Tenderness behind the lower part of your kneecap
The symptoms of jumper's knee may resemble other conditions or medical problems. Always see your healthcare provider for a diagnosis.
TREATMENT:
The best treatment for jumper's knee is to stop any activity that’s causing the problem until the injury is healed. Other treatment may include:
- Nonsteroidal anti-inflammatory medicines (NSAIDs, like ibuprofen or naproxen)
- Rest
- Elevating your knee
- Ice packs to your knee (to help reduce swelling)
- Stretching and strengthening exercises
- Patella tendon strap
Recommended Product(s):
> Patellofemoral Pain Syndrome (Runner’s Knee)
General Information
Patellofemoral pain syndrome is pain at the front of your knee, around your kneecap (patella). Sometimes called "runner's knee," it's more common in people who participate in sports that involve running and jumping.
The knee pain often increases when you run, walk up or down stairs, sit for long periods, or squat. Simple treatments — such as rest and ice — often help, but sometimes physical therapy is needed to ease patellofemoral pain.
SYMPTOMS:
These are the most common symptoms of runner's knee:
-
Pain in and around the kneecap that happens when you are active. Or pain after sitting for a long time with the knees bent. This sometimes causes weakness or feelings of instability.
-
Rubbing, grinding, or clicking sound of the kneecap that you hear when you bend and straighten your knee
-
Kneecap that is tender to the touch
TREATMENT:
Treatment of patellofemoral pain often begins with simple measures. Rest your knee as much as possible. Avoid or modify activities that increase the pain, such as climbing stairs, kneeling or squatting.
A physical therapist might suggest:
- Rehabilitation exercises.
- Supportive braces. Knee braces or arch supports may help improve pain.
- Taping. Your physical therapist may show you how to tape your knee to reduce pain and enhance your ability to exercise.
- Ice. Icing your knee after exercise might be helpful.
- Knee-friendly sports. Such as bicycling and swimming or water running.
If nonsurgical treatments aren't effective, your doctor might suggest:
- Arthroscopy.
- Realignment.
Recommended Product(s):
 B704 Stabilized Knee Support with Patellar Pad
B704 Stabilized Knee Support with Patellar Pad
 B720 Precision-fit Knee Support
B720 Precision-fit Knee Support
>> Read more about Patellofemoral Pain Syndrome in Mayoclinic.org for Anatomy / Description / Cause / Symptoms / Treatment.
> Knee Osteoarthritis
General Information
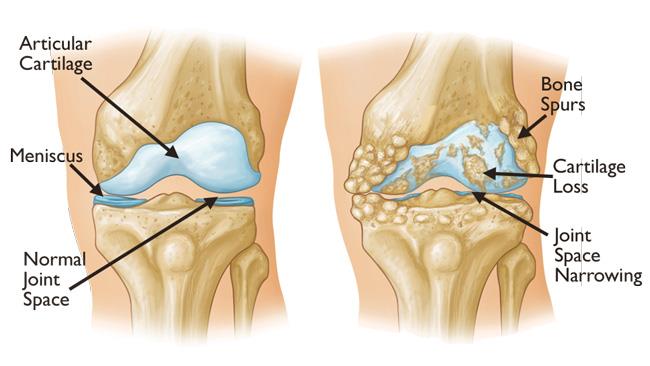
Osteoarthritis of the knee happens when the cartilage in your knee joint breaks down, enabling the bones to rub together. The friction makes your knees hurt, become stiff and sometimes swell. While osteoarthritis in the knee can’t be cured, there are many treatments to slow its progress and ease your symptoms. Surgery is an option for more severe forms of osteoarthritis.
Osteoarthritis of the knee is very common. Approximately 46% of people will develop it during their lifetimes.
Women are more likely than men to develop osteoarthritis of the knee. Most people develop this condition after age 40. But other factors such as injury or genetics can cause it to happen earlier.
Knee pain is the most common symptom of osteoarthritis in the knee, making it painful for you to jog, run, climb stairs or kneel. It can also make your knees feel stiff or swollen. Over time, osteoarthritis of the knee can change the shape of your knee joint, making your joint feel unstable or wobbly.
TREATMENT:
Treatment might include nonsurgical treatments, injections and surgery. Typically, healthcare providers try non-surgical treatments before recommending surgery.
Non-surgical treatments include:
- Using pain medications.
- Doing physical therapy.
- Maintaining a healthy weight.
- Using a knee brace.
- Using orthotics such as insoles or special footwear.
- Steroid injections.
- Viscosupplementation.
Surgical treatments include:
- Cartilage grafting. Healthy cartilage is used to fill a hole in your cartilage.
- Knee osteotomy.
- Partial knee replacement.
- Total rnee replacement.
Recommended Product(s):
 B704 Stabilized Knee Support with Patellar Pad
B704 Stabilized Knee Support with Patellar Pad  B720 Precision-fit Knee Support
B720 Precision-fit Knee Support
 B705 Premium Recovery Knee Brace
B705 Premium Recovery Knee Brace
 B709 Adjustable Knee Stabilizer
B709 Adjustable Knee Stabilizer
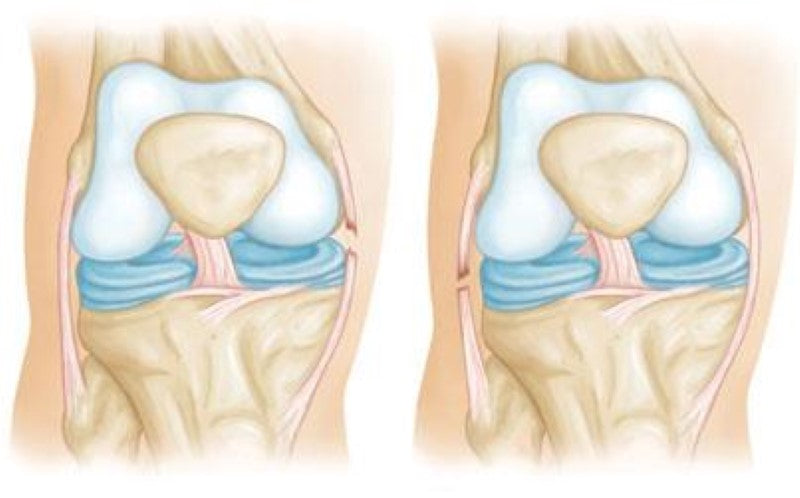
> Meniscus Tears

General Information
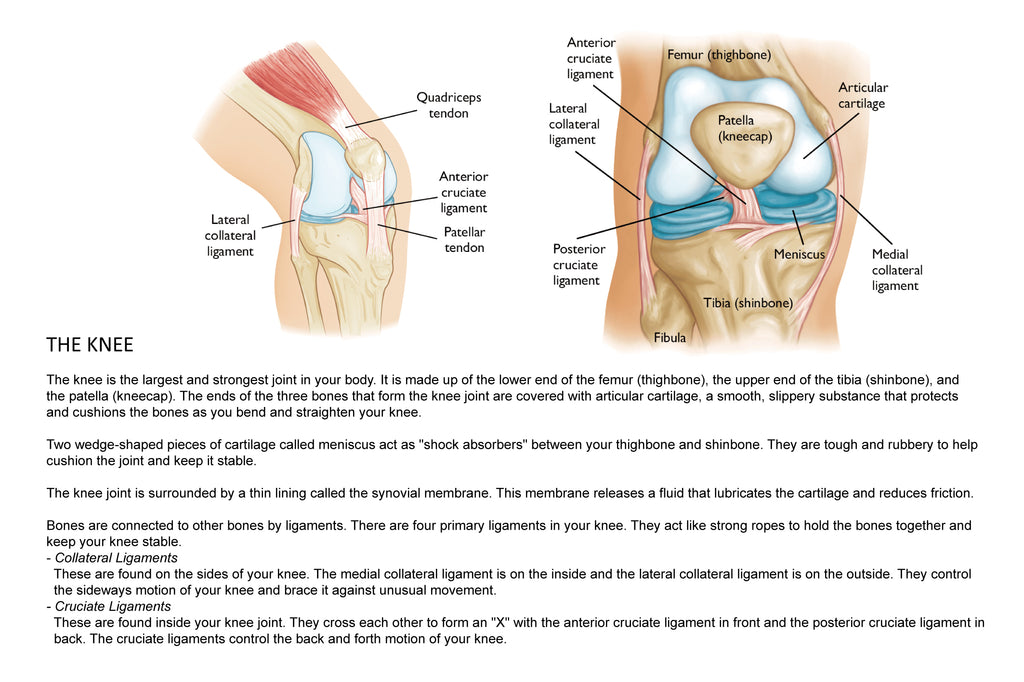
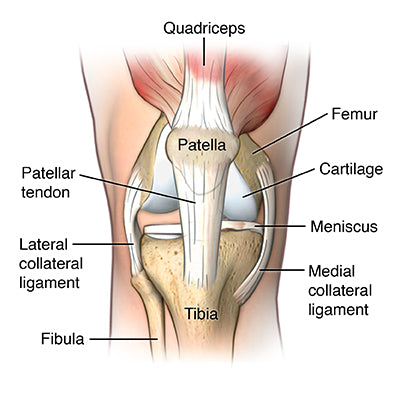
Two bones meet to form your knee joint: the femur and the tibia. The kneecap (patella) sits in front of the joint to provide some protection.
Two wedge-shaped pieces of fibrocartilage act as shock absorbers between your femur and tibia. These are the menisci. The menisci help to transmit weight from one bone to another and play an important role in knee stability.
The meniscus can tear from acute trauma or as the result of degenerative changes that happen over time. Tears are noted by how they look, as well as where the tear occurs in the meniscus. Common tears include bucket handle, flap, and radial.
The most common symptoms of a meniscus tear are:
- Pain
- Stiffness and swelling
- Catching or locking of your knee
- The sensation of your knee giving way
- Inability to move your knee through its full range of motion
TREATMENT:
Many meniscus tears will not need immediate surgery. If your symptoms do not persist and you have no locking or swelling of the knee, your doctor may recommend nonsurgical treatment.
- RICE. The RICE protocol is effective for most sports-related injuries. RICE stands for Rest, Ice, Compression, and Elevation.
- Rest. Take a break from the activity that caused the injury. Your doctor may recommend that you use crutches to avoid putting weight on your leg.
- Ice. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
- Compression. To prevent additional swelling and blood loss, wear an elastic compression bandage.
- Elevation. To reduce swelling, recline when you rest, and put your leg up higher than your heart.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Steroid injection.
- Other nonsurgical treatment.
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Recommended Product(s):
 B704 Stabilized Knee Support with Patellar Pad
B704 Stabilized Knee Support with Patellar Pad  B720 Precision-fit Knee Support
B720 Precision-fit Knee Support
 B705 Premium Recovery Knee Brace
B705 Premium Recovery Knee Brace
 B709 Adjustable Knee Stabilizer
B709 Adjustable Knee Stabilizer
>> Read more about Meniscus Tears in orthoinfo.aaos.org.com for Anatomy / Description / Cause / Symptoms / Treatment / Recovery.
> Osgood-Schlatter Disease (Knee Pain)

General Information
Osgood-Schlatter disease is a common cause of knee pain in growing adolescents. It is an inflammation of the area just below the knee where the tendon from the kneecap (patellar tendon) attaches to the shinbone (tibia).
The bones of children and adolescents possess a special area where the bone is growing called the growth plate. Growth plates are areas of cartilage located near the ends of bones. When a child is fully grown, the growth plates harden into solid bone.
Some growth plates serve as attachment sites for tendons, the strong tissues that connect muscles to bones. A bony bump called the tibial tubercle covers the growth plate at the end of the tibia. The group of muscles in the front of the thigh (called the quadriceps) attaches to the tibial tubercle.
When a child is active, the quadriceps muscles pull on the patellar tendon which, in turn, pulls on the tibial tubercle. In some children, this repetitive traction on the tubercle leads to inflammation of the growth plate. The prominence, or bump, of the tibial tubercle may become very pronounced.
Painful symptoms are often brought on by running, jumping, and other sports-related activities. In some cases, both knees have symptoms, although one knee may be worse than the other.
- Knee pain and tenderness at the tibial tubercle
- Swelling at the tibial tubercle
- Tight muscles in the front or back of the thigh
TREATMENT:
Treatment for Osgood-Schlatter disease focuses on reducing pain and swelling. This typically requires limiting exercise activity until your child can enjoy activity without discomfort or significant pain afterwards. In some cases, rest from activity is required for several months, followed by a strength conditioning program.
Your child's doctor may recommend additional treatment methods, including:
- Stretching exercises. Stretches for the front and back of the thigh (quadriceps and hamstring muscles) may help relieve pain and prevent the disease from returning.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Drugs like ibuprofen, aspirin, and naproxen reduce pain and swelling.
- Ice. Icing the inflamed area may reduce pain and swelling. Use cold packs for 20 minutes at a time, several times a day. Do not apply ice directly to the skin.
Recommended Product(s):
 B707 Open Patellar Knee Support
B707 Open Patellar Knee Support
 B704 Stabilized Knee Support with Patellar Pad
B704 Stabilized Knee Support with Patellar Pad
 B720 Precision-fit Knee Support
B720 Precision-fit Knee Support
 B705 Premium Recovery Knee Brace
B705 Premium Recovery Knee Brace
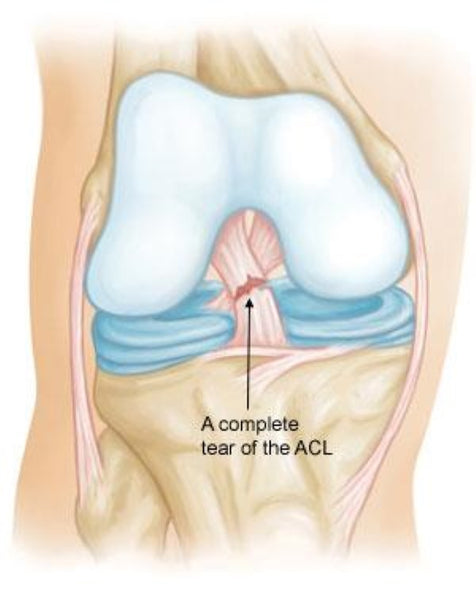
> Anterior Cruciate Ligament (ACL) Injuries
General Information
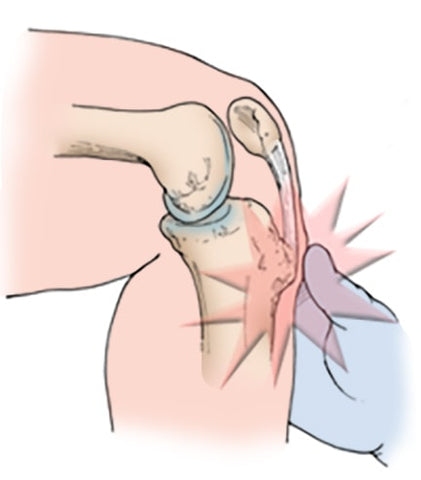
One of the most common knee injuries is an anterior cruciate ligament sprain or tear. Athletes who participate in high demand sports like soccer, football, and basketball are more likely to injure their anterior cruciate ligaments
The anterior cruciate ligament runs diagonally in the middle of the knee. It prevents the tibia from sliding out in front of the femur, as well as provides rotational stability to the knee.
About half of all injuries to the anterior cruciate ligament occur along with damage to other structures in the knee, such as articular cartilage, meniscus, or other ligaments.
When you injure your anterior cruciate ligament, you might hear a "popping" noise and you may feel your knee give out from under you. Other typical symptoms include:
- Pain with swelling.
- Loss of full range of motion
- Tenderness along the joint line
- Discomfort while walking
TREATMENT:
- Nonsurgical Treatment
A torn ACL will not heal without surgery. But nonsurgical treatment may be effective for patients who are elderly or have a very low activity level. If the overall stability of the knee is intact, your doctor may recommend simple, nonsurgical options.
- Bracing. Your doctor may recommend a brace to protect your knee from instability. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
- Physical therapy. As the swelling goes down, a careful rehabilitation program is started. Specific exercises will restore function to your knee and strengthen the leg muscles that support it.
- Surgical Treatment
Rebuilding the ligament. Most ACL tears cannot be sutured (stitched) back together. To surgically repair the ACL and restore knee stability, the ligament must be reconstructed. Your doctor will replace your torn ligament with a tissue graft. This graft acts as a scaffolding for a new ligament to grow on.
Recommended Product(s):
 B708 Adjustable Knee Brace with Side Stabilizers
B708 Adjustable Knee Brace with Side Stabilizers
 B709 Adjustable Knee Stabilizer
B709 Adjustable Knee Stabilizer
> Collateral Ligament Injuries
General Information
Athletes who participate in direct contact sports like football or soccer are more likely to injure their collateral ligaments.
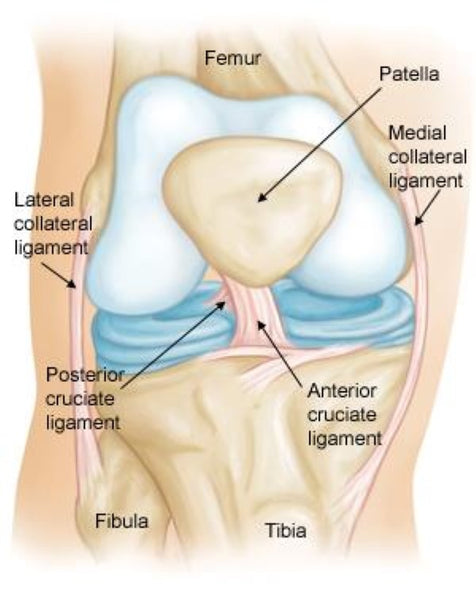
Bones are connected to other bones by ligaments. There are four primary ligaments in your knee. They act like strong ropes to hold the bones together and keep your knee stable.
Cruciate Ligaments. These are found inside your knee joint. They cross each other to form an X, with the anterior cruciate ligament in front and the posterior cruciate ligament in back. The cruciate ligaments control the front and back motion of your knee.
Collateral ligaments. These are found on the sides of your knee. They control the side to side motion of your knee and brace it against unusual movement.
- The medial collateral ligament (MCL) is on the inside. It connects the femur to the tibia.
- The lateral collateral ligament (LCL) is on the outside. It connects the femur to the fibula (the smaller bone in the lower leg).
Injured ligaments are considered sprains and are graded on a severity scale.
Grade 1 Sprains. The ligament is mildly damaged in a Grade 1 Sprain. It has been slightly stretched, but is still able to help keep the knee joint stable.
Grade 2 Sprains. A Grade 2 Sprain stretches the ligament to the point where it becomes loose. This is often referred to as a partial tear of the ligament.
Grade 3 Sprains. This type of sprain is most commonly referred to as a complete tear of the ligament. The ligament has been torn in half or pulled directly off the bone, and the knee joint is unstable.
The MCL is injured more often than the LCL. Due to the more complex anatomy of the outside of the knee, if you injure your LCL, you usually injure other structures in the joint, as well.
COMMON SYMPTOMS:
- Pain at the sides of your knee. If there is an MCL injury, the pain is on the inside of the knee; an LCL injury may cause pain on the outside of the knee.
- Swelling over the site of the injury.
- Instability — the feeling that your knee is giving way.
TREATMENT:
-
- Nonsurgical Treatment
Ice. Icing your injury is important in the healing process. The proper way to ice an injury is to apply crushed ice directly to the injured area for 15 to 20 minutes at a time, with at least 1 hour between icing sessions. Chemical cold products (blue ice) should not be placed directly on the skin and are not as effective.
Bracing. Your knee must be protected from the same sideway force that caused the injury. You may need to change your daily activities to avoid risky movements. Your doctor may recommend a brace to protect the injured ligament from stress. To further protect your knee, you may be given crutches to keep you from putting weight on your leg.
Physical therapy. Your doctor may suggest strengthening exercises. Specific exercises will restore function to your knee and strengthen the leg muscles that support it.
- Surgical Treatment
Most isolated collateral ligament injuries can be successfully treated without surgery. If the collateral ligament is torn in such a way that it cannot heal or is associated with other ligament injuries, your doctor may suggest surgery to repair it. Your surgeon will discuss which tecnique of repair is best for you.
Recommended Product(s):
 B709 Adjustable Knee Stabilizer
B709 Adjustable Knee Stabilizer
> Patellar Dislocation and Instability in Children (Unstable Kneecap)
General Information
Your child's kneecap (patella) is usually right where it should be—resting in a groove at the end of the thighbone (femur). When the knee bends and straightens, the patella moves straight up and down within the groove. Sometimes, the patella slides too far to one side or the other. When this occurs — such as after a hard blow or fall — the patella can completely or partially dislocate.
When the patella slips out of place — whether a partial or complete dislocation — it typically causes pain and loss of function. Even if the patella slips back into place by itself, it will still require treatment to relieve painful symptoms. Be sure to take your child to the doctor for a full examination to identify any damage to the knee joint and surrounding soft tissues.
In children with normal knee structure, patellar dislocations are often the result of a direct blow or a fall onto the knee. This incidence is more common in high-impact sports, such as football.
COMMON SYMPTOMS:
Some general symptoms your child may experience include:
- Pain
- Feeling the kneecap shift or slide out of the groove
- Feeling the knee buckle or give way
- Hearing a popping sound when the patella dislocates
- Swelling
- A change in the knee's appearance — the knee may appear misshapen or deformed
- Apprehension or fear when running or changing direction.
TREATMENT:
Nonsurgical Treatment
- Immobilization. Your doctor may recommend that your child wear a brace for 3 to 4 weeks. This stabilizes the knee while it heals.
- Weightbearing. Because putting weight on the knee may cause pain and slow the healing process, your doctor may recommend using crutches for the first week or two after the injury.
- Physical therapy.
Surgical Treatment
If your child's patella dislocates multiple times, or continues to be unstable despite therapy and bracing, surgery may be recommended to correct the problem. The type of surgery will depend on the cause of the unstable kneecap.
Recommended Product(s):
 B708 Adjustable Knee Brace with Side Stabilizers
B708 Adjustable Knee Brace with Side Stabilizers
 B709 Adjustable Knee Stabilizer
B709 Adjustable Knee Stabilizer
 B704 Stabilized Knee Support with Patellar Pad
B704 Stabilized Knee Support with Patellar Pad
 B720 Precision-fit Knee Support
B720 Precision-fit Knee Support