Elbow / Arm / Shoulder Injury Guide
COMMON INJURIES
> Recurrent and Chronic Elbow Instability

General Information
Elbow instability is a looseness in the elbow joint that may cause the joint to catch, pop, or slide out of place during certain arm movements. It most often occurs as the result of an injury — typically, an elbow dislocation. This type of injury can damage the bone and ligaments that surround the elbow joint.
When the elbow is loose and repeatedly feels as if it might slip out of place, it is called recurrent or chronic elbow instability.
There are three different types of recurrent elbow instability:
- Posterolateral rotatory instability. The elbow slides in and out of the joint due to an injury of the lateral collateral ligament complex, a soft tissue structure located on the outside of the elbow. This is the most common type of recurrent elbow instability. Associated fractures can also occur with this type of instability.
CAUSE: Typically caused by a trauma, such as a fall on an outstretched hand. It may also develop as a result of a previous surgery, or longstanding elbow deformity.
- Valgus instability. The elbow is unstable due to an injury of the medial collateral ligament, a soft tissue structure located on the inside of the elbow.
CAUSE: Valgus instability is most often caused by repetitive stress as seen in overhead athletes (such as baseball pitchers). Like the other forms of recurrent elbow instability, it may also result from a traumatic event.
- Varus posteromedial rotatory instability. The elbow slides in and out of the joint due to an injury of the lateral collateral ligament complex, in addition to a fracture of the coronoid portion of the ulna bone on the inside of the elbow.
CAUSE: Varus posteromedial rotatory instability is typically caused by a traumatic event, such as a fall.
TREATMENT:
Nonsurgical treatment options are effective at managing symptoms in most patients with valgus instability. However, a highly competitive overhead athlete who has a complete medial collateral ligament tear may require surgery to return to full function.
Nonsurgical management includes:
- Physical therapy. Specific exercises to strengthen the muscles around the elbow joint may improve symptoms.
- Activity modification. Symptoms may also be relieved by limiting activities that cause pain or feelings of instability.
- Bracing. A brace may help to limit painful movements and stabilize the elbow.
- Non-steroidal anti-inflammatory drugs (NDAIDs). Anti-inflammatory drugs like aspirin, ibuprofen, and naproxen may be helpful with pain during the initial injury.
Recommended Product(s):
 B305 Adjustable Elbow Support
B305 Adjustable Elbow Support  B320 Precision-fit Elbow Support
B320 Precision-fit Elbow Support  B303 Elastic Elbow Support
B303 Elastic Elbow Support
> Tennis Elbow (Lateral Epicondylitis)

General Information
Tennis elbow, or lateral epicondylitis, is a painful condition of the elbow caused by overuse. Not surprisingly, playing tennis or other racquet sports can cause this condition. However, several other sports and activities besides sports can also put you at risk.
Tennis elbow is inflammation or, in some cases, microtearing of the tendons that join the forearm muscles on the outside of the elbow. The forearm muscles and tendons become damaged from overuse — repeating the same motions again and again. This leads to pain and tenderness on the outside of the elbow.
SYMPTOMS:
Common signs and symptoms of tennis elbow include:
- Pain or burning on the outer part of your elbow
- Weak grip strength
- Sometimes, pain at night
The symptoms are often worsened with forearm activity, such as holding a racquet, turning a wrench, or shaking hands.
TREATMENT:
There are many treatment options for tennis elbow. In most cases, treatment involves a team approach. Primary doctors, physical therapists and, in some cases, surgeons work together to provide the most effective care.
Using a brace centered over the back of your forearm may also help relieve symptoms of tennis elbow. This can reduce symptoms by resting the muscles and tendons.
Recommended Product(s):
 B305 Adjustable Elbow Support
B305 Adjustable Elbow Support  B320 Precision-fit Elbow Support
B320 Precision-fit Elbow Support  B304 Tennis Elbow Strap
B304 Tennis Elbow Strap
> Elbow (Olecranon) Bursitis

General Information
Elbow bursitis occurs in the olecranon bursa, a thin, fluid-filled sac that is located at the boney tip of the elbow (the olecranon).
There are many bursae located throughout the body that act as cushions between bones and soft tissues, such as skin. They contain a small amount of lubricating fluid that allows the soft tissues to move freely over the underlying bone.
Normally, the olecranon bursa is flat. If it becomes irritated or inflamed, more fluid will accumulate in the bursa and bursitis will develop.
SYMTOMS:
Symptoms of elbow bursitis include :
- Swelling. The first symptom of elbow bursitis is often swelling. The skin on the back of the elbow is loose, which means that a small amount of swelling may not be noticed right away.
- Pain. As the swelling continues, the bursa begins to stretch, which causes pain. The pain often worsens with direct pressure on the elbow or with bending the elbow. The swelling may grow large enough to restrict elbow motion.
- Redness and warm to the touch. If the bursa is infected, the skin becomes red and warm. If the infection is not treated right away, it may spread to other parts of the arm or move into the bloodstream. This can cause serious illness. Occasionally, an infected bursa will open spontaneously and drain pus.
TREATMENT:
If the bursitis is not from an infection, there are several management options.
- Elbow pads. An elbow pad may be used to cushion your elbow.
- Activity changes. Avoid activities that cause direct pressure to your swollen elbow.
- Medications. Oral medications such as ibuprofen or other anti-inflammatories may be used to reduce swelling and relieve your symptoms.
If swelling and pain do not respond to these measures after 3 to 6 weeks, your doctor may recommend removing fluid from the bursa and injecting a corticosteroid medication into the bursa.
Recommended Product(s):
 B305 Adjustable Elbow Support
B305 Adjustable Elbow Support  B320 Precision-fit Elbow Support
B320 Precision-fit Elbow Support  B303 Elastic Elbow Support
B303 Elastic Elbow Support
> Radial Head Fractures of the Elbow

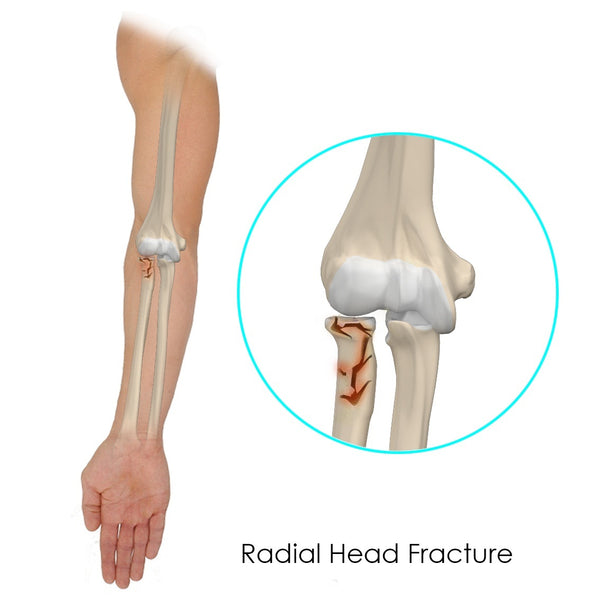
General Information
While trying to break a fall with your hands may seem instinctive, the force of the fall could travel up your forearm bones and dislocate your elbow. It also could break the smaller bone (radius) in your forearm. Fractures of the radius often occur in the part of the bone near the elbow, called the radial head.
Radial head fractures are common injuries, occurring in about 20% of all acute elbow injuries. Many elbow dislocations also involve fractures of the radial head.
COMMON SYMPTOMS:
The most common symptoms of a radial head fracture include:
- Pain on the outside of the elbow
- Swelling in the elbow joint
- Difficulty bending or straightening the elbow, accompanied by pain
- Inability to turn or difficulty turning the forearm (palm up to palm down or vice versa)
TREATMENT:
Doctors classify fractures according to the degree of displacement (how far out of normal position the bones are) and how many fragments there are. Treatment is determined by the type of fracture.
Type I fractures are generally small cracks, and the bone pieces remain fitted together. Nonsurgical treatment involves using a splint or sling for a few days, followed by an early and gradual increase in elbow and wrist movement (depending on the level of pain).
Type II fractures are slightly displaced and involve a larger piece of bone. If displacement is minimal, treatment may involve wearing a sling or splint for 1 to 2 weeks, followed by range-of-motion exercises.
Recommended Product(s):
 B403 Comfort Arm Sling
B403 Comfort Arm Sling  B305 Adjustable Elbow Support
B305 Adjustable Elbow Support  B404 Deluxe Shoulder Immobilizer
B404 Deluxe Shoulder Immobilizer
> Clavicle Fracture (Broken Collarbone)
General Information
A clavicle fracture is a break in the collarbone, one of the main bones in the shoulder. This type of fracture is fairly common, accounting for about 5% of all adult fractures.
Most clavicle fractures occur when a fall onto the shoulder or an outstretched arm puts enough pressure on the bone that it snaps or breaks. A broken collarbone can be very painful and can make it hard to move your arm. Other signs and symptoms of a fracture may include:
- Sagging of the shoulder downward and forward
- Inability to lift the arm because of pain
- A grinding sensation when you try to raise the arm
- A deformity or bump over the break
- Bruising, swelling, and/or tenderness over the collarbone
TREATMENT:
Many clavicle fractures can be treated by wearing a sling to keep the arm and shoulder from moving while the bone heals. With some clavicle fractures, however, the pieces of bone move far out of place when the injury occurs. For these more complicated fractures, surgery may be needed to realign the collarbone.
Recommended Product(s):
 B403 Comfort Arm Sling
B403 Comfort Arm Sling B404 Deluxe Shoulder Immobilizer
B404 Deluxe Shoulder Immobilizer
> Dislocated Shoulder
General Information
The shoulder joint is the body's most mobile joint. It can turn in many directions, but this advantage also makes the shoulder an easy joint to dislocate.
A partial dislocation (subluxation) means the head of the upper arm bone (humerus) is partially out of the socket (glenoid). A complete dislocation means it is all the way out of the socket. Both partial and complete dislocations cause pain and unsteadiness in the shoulder.
SYMPTOMS:
Symptoms of a dislocated shoulder include:
- Deformity
- Swelling
- Numbness
- Weakness
- Bruising
Sometimes a dislocation may tear ligaments or tendons in the shoulder or damage nerves.
TREATMENT:
For the treatment, your doctor will place the ball of the upper arm bone (humerus) back into the joint socket. This process is called a closed reduction. Severe pain stops almost immediately once the shoulder joint is back in place.
Your doctor may immobilize the shoulder in a sling or other device for several weeks following treatment. Plenty of early rest is needed. The sore area can be iced 3 to 4 times a day.
Recommended Product(s):
 B401 Adjustable Shoulder Support
B401 Adjustable Shoulder Support  B403 Comfort Arm Sling
B403 Comfort Arm Sling B404 Deluxe Shoulder Immobilizer
B404 Deluxe Shoulder Immobilizer
> Rotator Cuff Tears
General Information
A rotator cuff tear is a common cause of pain and disability among adults. Each year, almost 2 million people in the United States visit their doctors because of a rotator cuff problem.
Your arm is kept in your shoulder socket by your rotator cuff. The rotator cuff is a group of four muscles that come together as tendons to form a covering around the head of the humerus. The rotator cuff attaches the humerus to the shoulder blade and helps to lift and rotate your arm.
When one or more of the rotator cuff tendons is torn, the tendon no longer fully attaches to the head of the humerus.Most tears occur in the supraspinatus tendon, but other parts of the rotator cuff may also be involved.
In many cases, torn tendons begin by fraying. As the damage progresses, the tendon can completely tear, sometimes with lifting a heavy object.
SYMPTOMS:
The most common symptoms of a rotator cuff tear include:
- Pain at rest and at night, particularly if lying on the affected shoulder
- Pain when lifting and lowering your arm or with specific movements
- Weakness when lifting or rotating your arm
- Crepitus or crackling sensation when moving your shoulder in certain positions
TREATMENT:
In about 80% of patients, nonsurgical treatment relieves pain and improves function in the shoulder.
Nonsurgical treatment options may include:
- Rest. Your doctor may suggest rest and limiting overhead activities. He or she may also prescribe a sling to help protect your shoulder and keep it still.
- Activity modification. Avoid activities that cause shoulder pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Anti-inflammatory drugs like ibuprofen, aspirin, and naproxen reduce pain and swelling.
- Strengthening exercises and physical therapy.
- Steroid injection.
Recommended Product(s):
 B401 Adjustable Shoulder Support
B401 Adjustable Shoulder Support  B403 Comfort Arm Sling
B403 Comfort Arm Sling B404 Deluxe Shoulder Immobilizer
B404 Deluxe Shoulder Immobilizer





