Ankle / Foot Injury Guide
COMMON INJURIES
> Sprained Ankle
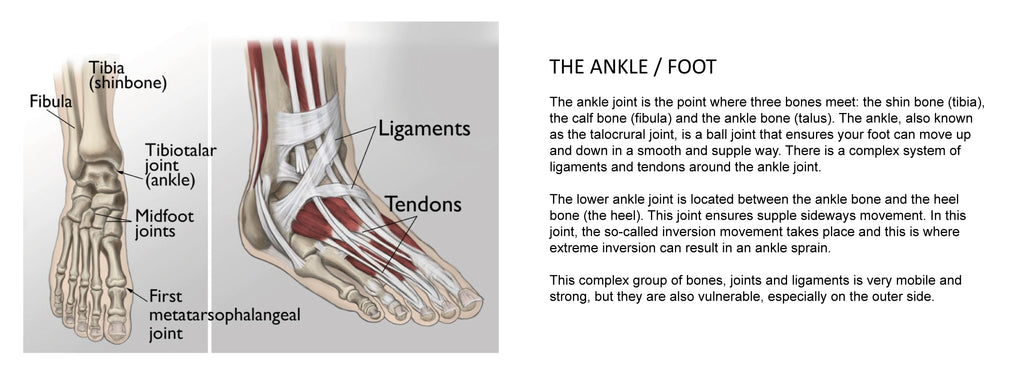
General Information
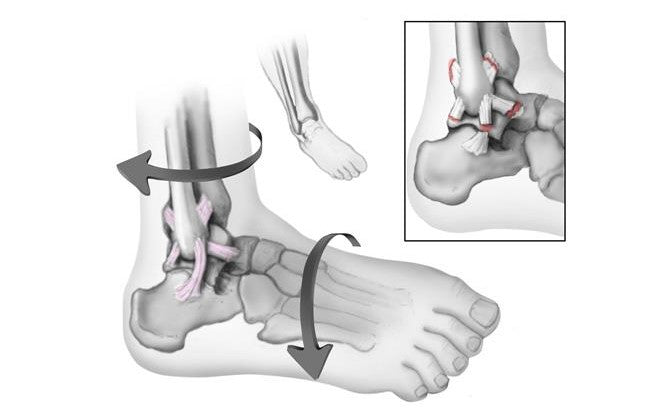
An ankle sprain occurs when the strong ligaments that support the ankle stretch beyond their limits and tear. Ankle sprains are common injuries that occur among people of all ages. They range from mild to severe, depending upon how much damage there is to the ligaments.
Most sprained ankles occur in the lateral ligaments on the outside of the ankle. Sprains can range from tiny tears in the fibers that make up the ligament to complete tears through the tissue.
COMMON SYMPTOMS:
A sprained ankle is painful. Other symptoms may include:
- Swelling
- Bruising
- Tenderness to touch
- Instability of the ankle—this may occur when there has been complete tearing of the ligament or a complete dislocation of the ankle joint.
If there is severe tearing of the ligaments, you might also hear or feel a "pop" when the sprain occurs. Symptoms of a severe sprain are similar to those of a broken bone and require prompt medical evaluation.
TREATMENT:
Nearly all isolated low ankle sprains can be treated without surgery. Even a complete ligament tear (Grade 3) will heal without surgical repair if it is immobilized and rehabilitated appropriately.
A three-phase program guides treatment for all ankle sprains — from mild to severe:
Phase 1
- Includes a short period of immobiliztion, rest, and ice to reduce the swelling.
- Early weightbearing as tolerated is typically recommended during this phase.
- For a Grade 2 sprain, a removable plastic device, such as a walking boot or cast-brace, can provide support.
- Grade 3 sprains may require a short leg cast or cast-brace for 10 to 14 days.
- In most cases, swelling and pain will last 2 to 3 days. Walking may be difficult during this time, and your doctor may recommend that you use crutches as needed.
Phase 2
- Is typically initiated early and includes functional rehabilitation that focuses on:
- Range of motion exercises
- Isometric strengthening
- Proprioception (balance) retraining exercises
- It is important to discontinue ankle immobilization during this phase to avoid stiffness.
Phase 3
- Includes advancement of strengthening and proprioception exercises and the gradual return to pre-injury activities.
- Early return to sporting and work activities may require ankle taping or bracing.
This three-phase treatment program may take just 2 weeks to complete for minor sprains, or up to 6 to 12 weeks for more severe injuries.
Home Treatments
For milder sprains, your doctor may recommend simple home treatment.
The RICE protocol. Follow the RICE protocol as soon as possible after your injury:- Rest your ankle by not walking on it or returning to sport.
- Ice should be immediately applied to keep the swelling down. It can be used for 20 to 30 minutes, three or four times daily. Do not apply ice directly to your skin.
- Compression dressings, bandages, or ace-wraps will immobilize and support your injured ankle. The compression may also help with swelling.
- Elevate your ankle above the level of your heart as often as possible during the first 48 hours. Elevation also helps control the swelling.
Recommended Product(s):
 B904 Elastic Ankle Support
B904 Elastic Ankle Support  B906 Adjustable Ankle Support with figure 8 strap
B906 Adjustable Ankle Support with figure 8 strap  B920 Precision-fit Ankle Brace
B920 Precision-fit Ankle Brace  B908 Lace-up Ankle Stabilizer
B908 Lace-up Ankle Stabilizer  B909 Sports Ankle Brace with Cross Straps
B909 Sports Ankle Brace with Cross Straps
> Ankle Fractures (Broken Ankle)
General Information
A broken ankle is also known as an ankle "fracture." This means that one or more of the bones that make up the ankle joint are broken.
A fractured ankle can range from a simple break in one bone, which may not stop you from walking, to several fractures, which forces your ankle out of place and may require that you not put weight on it for a few months. Simply put, the more bones that are broken, the more unstable the ankle becomes. There may be ligaments damaged as well. The ligaments of the ankle hold the ankle bones and joint in position.
Doctors classify ankle fractures according to the area of bone that is broken. For example, a fracture at the end of the fibula is called a lateral malleolus fracture, or if both the tibia and fibula are broken, it is called a bimalleolar fracture.
SYMPTOMS:
Because a severe ankle sprain can feel the same as a broken ankle, every ankle injury should be evaluated by a physician.
Common symptoms for a broken ankle include:
- Immediate and severe pain
- Swelling
- Bruising
- Tender to touch
- Cannot put any weight on the injured foot
- Deformity ("out of place"), particularly if the ankle joint is dislocated as well
TREATMENT:
If the fracture is not out of place or is a very low fracture with very small pieces, it can be treated without surgery.
A stress x-ray may be done to see if the fracture and ankle are stable.
The fracture may be treated with a short leg cast or a removable brace. Usually, you need to avoid putting weight on your leg for approximately 6 weeks.
You will need to see your physician regularly for repeat x-rays to make sure the fracture does not change in position.
If the fracture is out of place or the ankle is unstable, surgery may be recommended.
In some cases, surgery may be considered even if the fracture is not out of place. This is done to reduce the risk of the fracture not healing (called a nonunion), and to allow you to start moving the ankle earlier.
Supports / Braces
It is very common to have several different kinds of things to wear on the injured ankle, depending on the injury.
Initially, most ankle fractures are placed in a splint to protect your ankle and allow for the swelling to go down. After that, you may be put into a cast or removable brace.
Even after the fracture has healed, your physician may recommend wearing an ankle brace for several months while you are doing sporting activities.
Recommended Product(s):
 B908 Lace-up Ankle Stabilizer
B908 Lace-up Ankle Stabilizer  B909 Sports Ankle Brace with Cross Straps
B909 Sports Ankle Brace with Cross Straps
>> Read more about Ankle Fractures in Orthoinfo.aoos.org for Anatomy / Description / Cause / Symptoms / Treatment / Recovery.
> Achilles Tendinitis
General Information
Achilles tendinitis is a common condition that occurs when the large tendon that runs down the back of the lower leg becomes irritated and inflamed.
The Achilles tendon is the largest tendon in the body. It connects the calf muscles to the heel bone and is used when you walk, run, climb stairs, jump, and stand on your tip toes. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse.
There are two types of Achilles tendinitis, based on which part of the tendon is inflamed: Noninsertional Achilles Tendinitis and Insertional Achilles Tendinitis. The two types can occur separately or at the same time
Achilles tendinitis is typically not related to a specific injury. The problem results from repetitive stress to the tendon. This often happens when we push our bodies to do too much, too quickly.
COMMON SYMPTOMS:
Common symptoms of Achilles tendinitis include:
- Pain and stiffness along the Achilles tendon in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Severe pain the day after exercising
- Thickening of the tendon
- Bone spur formation (insertional tendinitis)
- Swelling that is present all the time and gets worse throughout the day or with activity
- Pain on the back of the heal when you wear shoes
TREATMENT:
In most cases of Achilles tendinitis, nonsurgical treatment options will provide adequate pain relief, although it may take a few months for symptoms to completely subside. Even with early treatment, the pain may last longer than 3 months.
Non-surgical treatments include:
- Rest.
- Ice.
- Non-steroidal Anti-inflammatory Drugs (NSAIDs).
- Physical Therapy.
- Cortisone Injections.
- Night Splinting.
- Supportive Shoes and Orthotics
Recommended Product(s):
 B904 Elastic Ankle Support
B904 Elastic Ankle Support  B906 Adjustable Ankle Support with figure 8 strap
B906 Adjustable Ankle Support with figure 8 strap  B920 Precision-fit Ankle Brace
B920 Precision-fit Ankle Brace
> Plantar Fasciitis and Bone Spurs

General Information
Plantar fasciitis is the most common cause of pain on the bottom of the heel. Approximately 2 million patients are treated for this condition every year.
The plantar fascia is a long, thin ligament that lies directly beneath the skin on the bottom of your foot. It connects the heel to the front of your foot, and supports the arch of your foot. Plantar fasciitis occurs when this strong band of tissue that supports the arch of your foot becomes irritated and inflamed.
COMMON SYMPTOMS:
The most common symptoms of plantar fasciitis include:
- Pain on the bottom of the foot near the heel
- Pain with the first few steps after getting out of bed in the morning, or after a long period of rest, such as after a long car ride. The pain subsides after a few minutes of walking
- Greater pain after (not during) exercise or activity
TREATMENT:
More than 90% of patients with plantar fasciitis will improve within 10 months of starting simple treatment methods.
- Rest. Decreasing or even stopping the activities that make the pain worse is the first step in reducing the pain. You may need to stop athletic activities where your feet pound on hard surfaces (for example, running or step aerobics).
- Ice. Rolling your foot over a cold water bottle or ice for 20 minutes is effective. This can be done 3 to 4 times a day.
- Nonsteroidal anti-inflammatory medication.
- Exercise. Plantar fasciitis is aggravated by tight muscles in your feet and calves. Stretching your calves and plantar fascia is the most effective way to relieve the pain that comes with this condition.
- Cortisone injections.
- Supportive shoes and orthotics.
-Night splints. Most people sleep with their feet pointed down. This relaxes the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be difficult to sleep with, a night splint is very effective and does not have to be used once the pain is gone.
- Physical therapy. Your doctor may suggest that you work with a physical therapist on an exercise program that focuses on stretching your calf muscles and plantar fascia.
- Extracorporeal shockwave therapy (ESWT).
If your symptoms persist with nonsurgical treatment, your doctor may suggest arthroscopic surgery.
Recommended Product(s):
 B904 Elastic Ankle Support
B904 Elastic Ankle Support  B906 Adjustable Ankle Support with figure 8 strap
B906 Adjustable Ankle Support with figure 8 strap  B920 Precision-fit Ankle Brace
B920 Precision-fit Ankle Brace  B905 Adjustable Ankle Support
B905 Adjustable Ankle Support

